Vivace® Direct – February 16th, 2024
A Clinician’s Approach: An Individual Case Study Using Vivace Ultra™ on the Arms
By Anna Mkrtchyan, NMD
Anna Mkrtchyan is the Founder and Owner of Glam Doctor Corporation. She have been a physician in the aesthetics industry since 2013 and with each patient, she always find small nuances that help her to individualize the approach to treating each case. The constant evolution of this industry yields new technologies to further personalize treatments such as industry-first ultrasound to visualize dermal and epidermal depths with the Vivace Ultra™ Uniform Radiofrequency Microneedling. As these advances become available, providers can give each patient a unique experience.

A post-menopausal patient with an active lifestyle and substantial life experience visited my office with the goal of improving the appearance of her arms. Despite maintaining a consistent weightlifting routine focused on toning the skin, especially in the arms (partly due to genetics), she faced challenges in reducing laxity and excess adipose tissue. The patient was not open to surgical intervention.
1. The consultation began with a discussion of the patient’s primary goals for optimizing her arms’ appearance. The patient expressed a desire for both skin tightening and adipose reduction, with a particular focus on addressing the inferior portion that seemed to exert a downward pull on her skin and make it appear more loose.
2. We set clear expectations and discussed the possibility of exploring alternative treatment paths, such as surgical options. The patient did not want to consider surgery as an option altogether. She understood that multiple Vivace Ultra™ treatments would be necessary to see optimal results. Additionally, she acknowledged that achieving final results would require time, given the gradual processes of neocollagenesis and elastin production. The patient was also aware of the financial commitments involved, understanding that additional treatments might be necessary to achieve a result that would fully satisfy her. Furthermore, she understood that the outcomes might never reach a level equivalent to a “surgical status.”
We conducted a comprehensive intake and review of her medical history to identify and eliminate any obvious contraindications and factors that might impact dermal/epidermal thickness. The patient exhibited no contraindications. During the discussion of ethnicity, she was classified as a Fitzpatrick Skin Type III and denied any history of post-inflammatory hyperpigmentation (PIH). Consequently, my inclination to pre-treat with a hydroquinone-based product diminished, as I generally prefer to use a non-insulated needle array whenever possible..
3. I identified treatment spacing, the preferred needle array type, and depth settings using the ultrasound handpiece on the device. Since she is post-menopausal, I decided to space her treatments slightly further apart to allow for adequate healing time on the body as well as maximizing the time the fibroblasts can “re-train” to begin producing collagen and elastin. I presented a treatment plan of three (3) treatments but did inform her that she may need up to six (6) treatments based on her expectations and the severity of skin laxity/subcutaneous adipose tissue present. I opted for the 60 non-Insulated needle array to maximize treatment area and address both concerns of skin laxity and adipose reduction. I also selected the 0.5MHz frequency to treat this body part.
4. Her ultrasound readings included a total epidermal + dermal depth reading of 1.5mm. I used only a topical benzocaine, lidocaine, tetracaine (BLT) compounded topical anesthetic of 20%/10%/10% concentration with plastic wrap for containment purposes. After 45 minutes, sufficient analgesia was achieved, and I began treatment. I opted to set my treatment depth at 2.5mm. My goal was to optimize treatment outcomes, acknowledging that a circumferential approach in the area would lead to circumferential reduction. Consequently, I delineated and treated the area from the antecubital fossa to the axillary hair and from just superior of the olecranon to the glenohumeral joint.
5. I assessed clinical endpoints and successfully concluded the first treatment. As the patient expressed a desire for rejuvenation, I examined for moderate amounts of erythema and edema in the test pulse areas. Optimal clinical endpoint reactions were observed at RF Power 5. The patient exhibited high tolerance throughout the procedure and after evaluating pain tolerance scales, the RF time was determined to be 500ms. I conducted only one pass per side with a 50% overlap since I was using a non-insulated needle array and completed approximately 850 pulses per arm.
6. Upon completion of the treatment, we discussed post care and expectations. I then applied Boost Serum to the treatment area bilaterally and thoroughly discussed post-care instructions, which includes avoiding direct sunlight and applying sunscreen liberally and often starting 24 hours after treatment. I reminded the patient to use clean bedsheets and not allow her pets to lick the treatment area. Additionally, I instructed the patient to apply the Boost Serum several times a day over the next few days and avoid any exfoliating products in the area. I reiterated to the patient that some patients may experience some redness, swelling, micro-crusting and pinpoint darkened pigmentation for up to two (2) weeks.
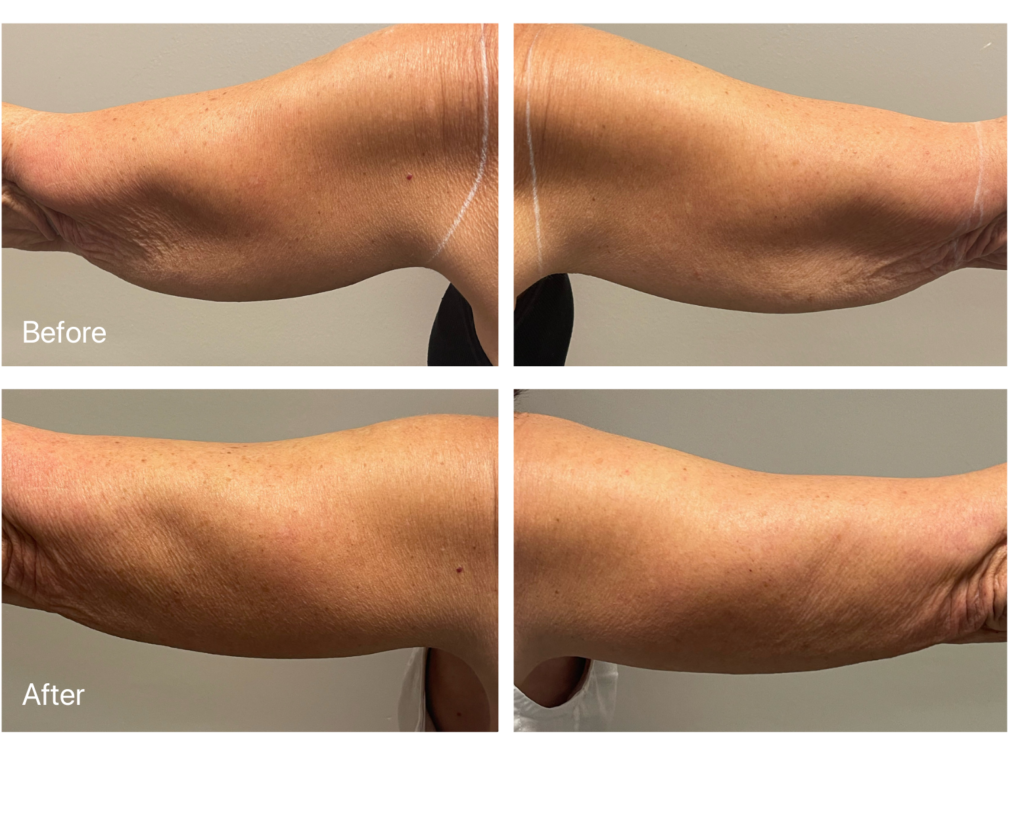
The patient returned six (6) weeks later, and we repeated the process. The results from the two treatments thus far, as indicated in the before and after photos, have demonstrated a visible improvement. While each patient and treatment situation is unique, the ability to comprehend the intricacies of each patient and effectively employ the tools available in this constantly evolving industry helps us maximize patient results
Get In Touch
